Groups with 25 or more clinicians participating in mips who are registered and choose to submit data using the cms web interface must report all 15 required quality measures for the full year january 1 december 31 2017.
Mips quality measures 2017.
Explore measures activities.
Systemic antimicrobial therapy avoidance of inappropriate use.
2017 mips quality measures.
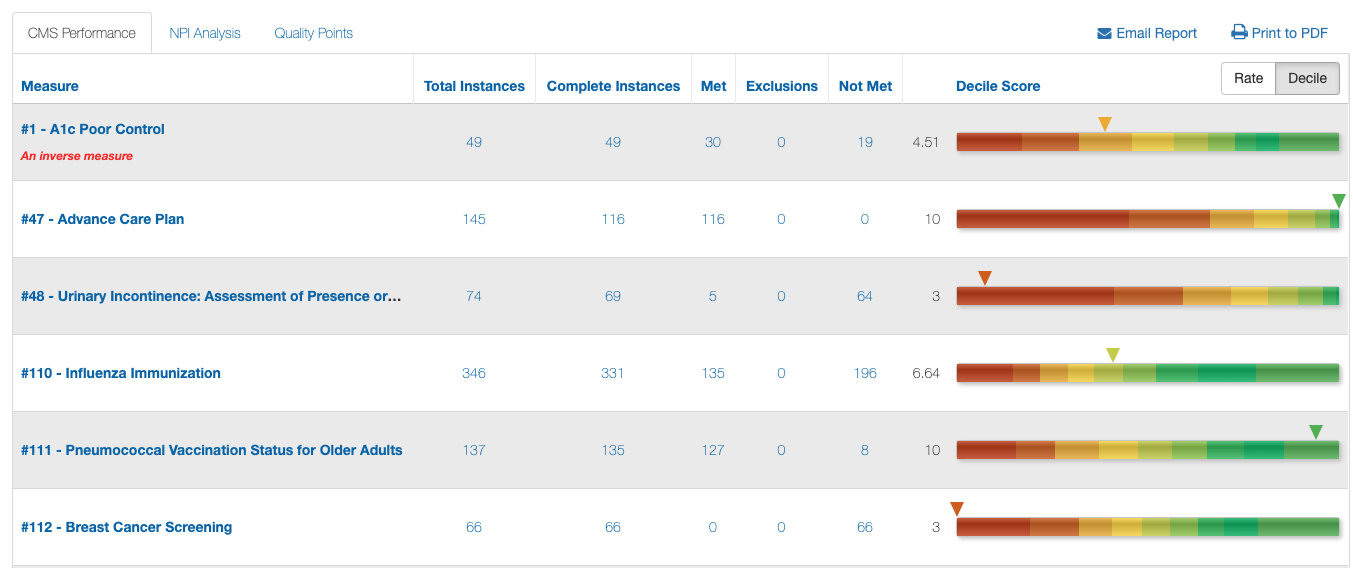
Unique to the 2017 transition reporting year the first year of the mips program cms is allowing a minimum floor of three points for all quality measures submitted.
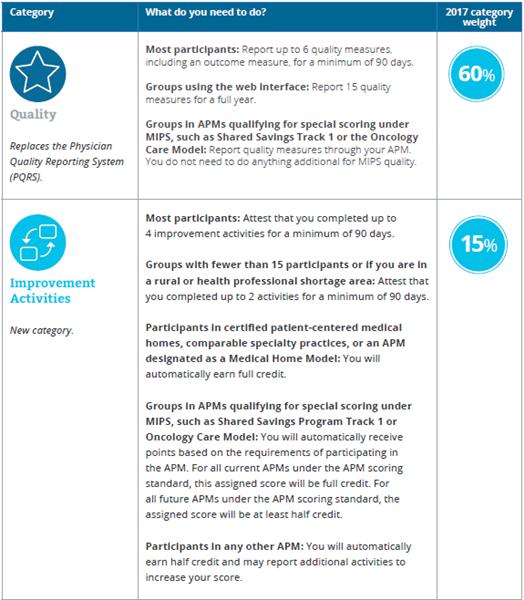
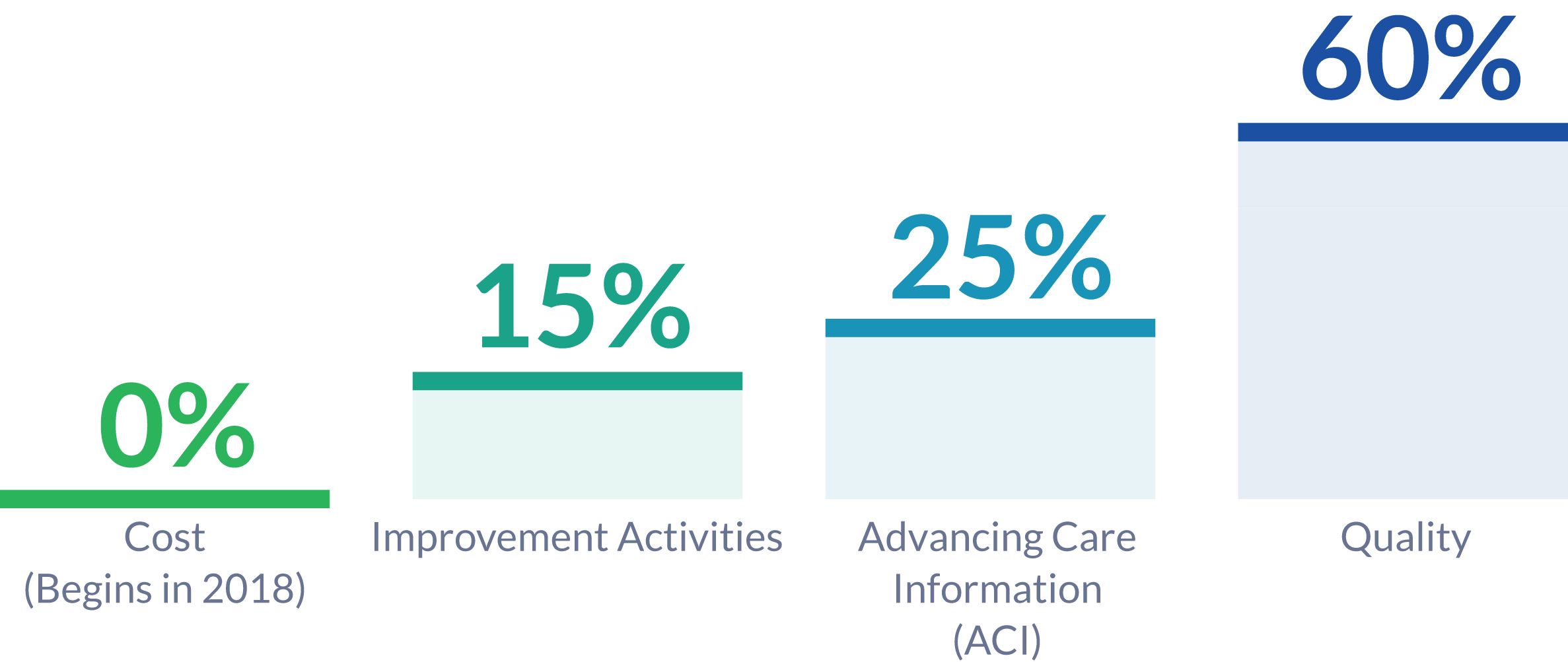
Streamlines multiple quality programs under the new merit based incentive payments system mips gives bonus payments for participation in eligible alternative payment models apms macra also required us to remove social security numbers ssns from all medicare cards by april 2019.
For ecs participating in mips apms the low volume threshold lvt is calculated at the apm entity level also referred to as the aco level.
Quality 45 of total score.
Acute otitis externa aoe.
2020 medicare part b claims measure specifications and supporting documents zip 2020 cms web interface measure specifications and supporting documents zip 2020 quality benchmarks zip 2020 clinical quality measure specifications and supporting documents zip 2020 mips quality measures list xlsx 2020 qcdr measure specifications xlsx.
Suggestions for your specialty include but are.
Small practices less than 16 in the practice can earn 3 points on a measure if at least 1 eligible case is reported.
This means that even if a clinician or group is at or below the low volume threshold of 30 000 in covered professional services under the medicare pfs or furnishing covered professional services to less than or.
Participants must submit collected data for 4 or 5 base score measures depending on the cehrt edition during 2017.
Special rules for the 2017 transition reporting year.
Report 6 measures including one outcome or other high priority measure for 12 months on at least 70 of eligible encounters to possibly earn more than 3 points on a measure.
A clinician or group participating in mips may submit a quality payment program hardship exception application citing one of the following specified reasons for review and.
Jump to 2019 mips quality measures quality id measure name high priority measure type details measure description full specifications.